Introduction
In the realm of women’s health, both urinary tract infections (UTIs) and menstrual cycles are topics that garner significant attention. However, it might come as a surprise that these seemingly unrelated issues could potentially interact.
UTIs and periods are two distinct bodily processes, but there exists a complex interplay between them that is worth exploring.
This blog post delves into the intriguing question: Can a UTI affect your period? Let’s uncover the surprising connections and shed light on this important aspect of women’s well-being. We will also explore the role of relevant lab tests in diagnosing and managing UTIs in the context of the menstrual cycle.
The Basics of UTIs and Menstrual Cycles
Before diving into their potential relationship and the role of lab tests, let’s review the basics of UTIs and menstrual cycles.
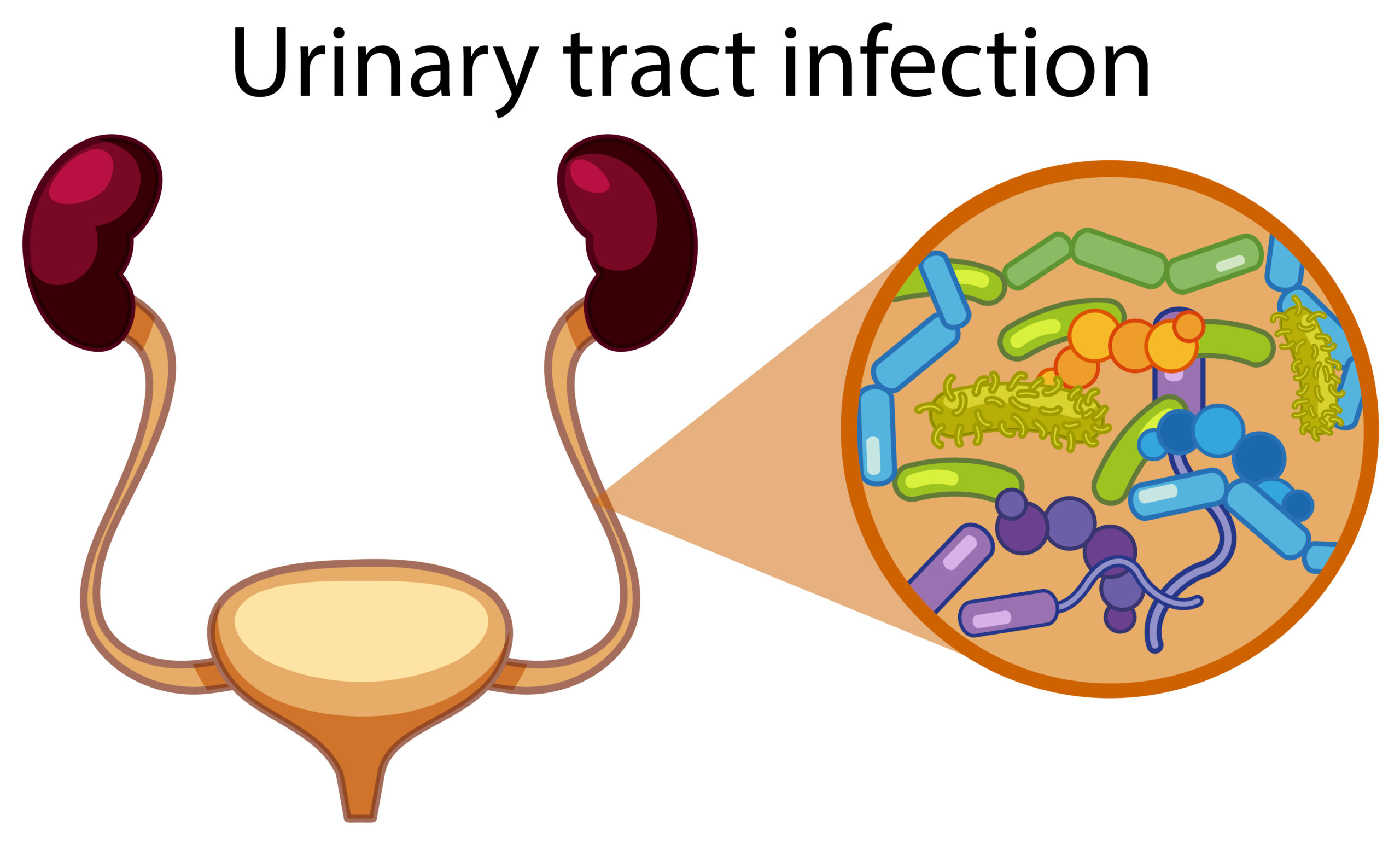
A urinary tract infection (UTI) is a bacterial infection that occurs in any part of the urinary system, which includes the bladder, urethra, ureters, and kidneys. Common symptoms of UTIs include a frequent urge to urinate, a burning sensation while urinating, cloudy or strong-smelling urine, and pelvic pain.
On the other hand, the menstrual cycle is a regular physiological process that occurs in females of reproductive age. It involves the shedding of the uterine lining, resulting in menstrual bleeding. The cycle typically lasts around 28 days, but it can vary for each individual.
The Interplay: Can a UTI Affect Your Period?
While UTIs and menstrual cycles primarily involve different bodily systems, there is evidence to suggest that they can influence each other in certain ways. To better understand this relationship, it’s crucial to explore how lab tests can aid in diagnosing and managing UTIs.
- Hormonal Fluctuations: Hormones play a crucial role in both UTIs and menstrual cycles. During menstruation, hormonal changes can impact the urinary tract, potentially making it more susceptible to infections. Similarly, hormonal fluctuations might affect the pH balance of the urinary tract, creating an environment conducive to bacterial growth.
- Lab Tests: To evaluate hormonal imbalances, tests such as blood hormone levels, including estrogen and progesterone, can be conducted. These tests can help identify whether hormonal fluctuations are contributing to UTIs.
- Pelvic Congestion: Menstruation can lead to increased blood flow to the pelvic region, causing congestion. This congestion might indirectly impact the urinary tract and potentially exacerbate UTI symptoms or increase the risk of infection.
- Lab Tests: In cases where pelvic congestion is suspected, diagnostic imaging such as ultrasound or MRI can be used to assess blood flow and congestion in the pelvic region.
- Immune Response: The immune system plays a pivotal role in combating both UTIs and infections. During menstruation, the immune system might be temporarily compromised, which could potentially influence the body’s ability to fight off UTI-causing bacteria.
- Lab Tests: To evaluate immune system health and response, blood tests like a complete blood count (CBC) can be performed. A CBC measures the levels of different blood components, including white blood cells, which are integral to the immune response.
- Hygiene Practices: Proper hygiene practices are crucial for preventing both UTIs and menstrual-related infections. During menstruation, maintaining hygiene becomes even more important, as improper practices could introduce harmful bacteria into the urinary tract, increasing the risk of infection.
- Lab Tests: In the context of hygiene practices, there are no specific lab tests, but urinary analysis can be used to detect the presence of bacteria and infection in the urinary tract.
- Overlapping Symptoms: Some symptoms of UTIs, such as pelvic discomfort and lower abdominal pain, can mimic menstrual cramps. This overlap in symptoms might lead to confusion, making it essential to accurately diagnose and treat the underlying issue
- Lab Tests: To differentiate between UTI symptoms and menstrual discomfort, urine cultures are often conducted. These tests can identify the specific bacteria causing the infection, helping healthcare professionals tailor treatment.
Managing UTIs and Periods
If you suspect that a UTI is affecting your period or vice versa, it’s crucial to seek medical advice. A healthcare professional can provide accurate diagnosis and recommend appropriate treatment options, including lab tests when necessary.
To manage both UTIs and periods effectively:
- Stay Hydrated: Drinking plenty of water can help flush out bacteria from the urinary tract and maintain overall health.
- Maintain Hygiene: During menstruation, practice good hygiene to prevent the introduction of harmful bacteria.
- Wear Breathable Clothing: Wearing breathable underwear and avoiding tight-fitting clothes can help maintain proper airflow and reduce the risk of bacterial growth.
- Urinate Regularly: Don’t hold in urine for extended periods, as this can increase the risk of UTIs.
Lab Tests in UTI Diagnosis and Management
Laboratory tests are invaluable tools for diagnosing and managing UTIs. These tests help healthcare professionals determine the presence of infection, identify the responsible bacteria, and assess the severity of the condition. Here are some of the key lab tests used in the context of UTIs:
- Urine Analysis: Urine Analysis is one of the most common tests for UTIs. A sample of your urine is examined to check for the presence of white blood cells, red blood cells, and bacteria. Abnormal levels of these components can indicate an infection.
- Urine Culture: A urine culture is performed when a UTI is suspected. It involves growing bacteria from a urine sample in a laboratory dish to identify the specific strain causing the infection. This helps in determining the most effective antibiotic for treatment.
- Complete Blood Count (CBC): As mentioned earlier, a CBC can assess the overall health of your immune system. If your white blood cell count is elevated, it may indicate an active infection.
- C-reactive Protein (CRP) Test: CRP is a marker of inflammation in the body. Elevated CRP levels can suggest the presence of an infection.
- Imaging: In severe or recurrent UTIs, imaging tests like ultrasound, CT scans, or MRI scans may be used to visualize the urinary tract and identify any structural abnormalities or obstructions.
Laboratory tests, along with a thorough medical history and physical examination, help healthcare providers make an accurate diagnosis and develop a personalized treatment plan.
Conclusion:
In the intricate landscape of women’s health, the connection between UTIs and menstrual cycles might not be immediately apparent, but it’s important to recognize their potential influence on each other. Hormones, immune responses, and hygiene practices all play roles in this interplay. Remember, maintaining good hygiene, staying hydrated, and seeking medical attention when needed are essential steps to ensure both your urinary tract and menstrual cycle remain in optimal health. Lab tests are vital tools in the diagnosis and management of UTIs, helping healthcare professionals provide the most effective care for your specific situation. If you ever experience unusual changes in your menstrual cycle or persistent UTI symptoms, consult a healthcare professional to ensure your well-being and address any potential issues effectively.
Other Health Articles:
Understanding the Causes of Vulvar Pain During Your Menstrual Cycle
Irregular Periods: Why Is My Period Late? 11 possible reasons
5 Safe and Effective Ways to Start Your Period Naturally: Methods and Risks Explained
Natural Solutions to Prevent Pregnancy After a Missed Period
Disclaimers:
Medical Advice: The information provided in this blog post is for educational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional for personalized guidance regarding your specific medical condition.
Accuracy of Information: While we strive to provide accurate and up-to-date information, the field of medicine and viral fevers is constantly evolving. The content in this blog post may not reflect the most current research or medical guidelines. Therefore, it is advisable to cross-check any information provided with reliable sources or consult a healthcare professional.
Individual Variations: The symptoms, causes, treatment options, and preventive measures discussed in this blog post are general in nature and may not apply to everyone. It is important to remember that each individual’s situation is unique, and personalized medical advice should be sought when making healthcare decisions.
External Links: This blog post may contain links to external websites or resources for additional information. However, we do not endorse or have control over the content of these third-party websites. Accessing these links is done at your own risk, and we are not responsible for any consequences or damages that may arise from visiting these external sources.
Results May Vary: The effectiveness of treatment options or preventive measures mentioned in this blog post may vary from person to person. What works for one individual may not work the same way for another. It is essential to consult with a healthcare professional for personalized advice tailored to your specific needs.